Addiction

Written by:

Medically Reviewed by:
Last Updated:
October 13th, 2025
Ask an addiction specialist to define addiction, and chances are the reply would begin with, “How long have you got?” Addiction is complicated because it doesn’t look the same for everyone. What drags one person down might barely register for another, which is why it resists a neat definition.
The reality is that addiction is highly complex. What we can do is lay the groundwork by exploring how addiction can begin, why it tightens its grip, and what makes it so difficult to walk away from. Most importantly, we can help you take the next step toward getting the right support, whether that’s for yourself or someone close to you.
What exactly is an addiction?
We use the word ‘addiction’ so casually these days. I’m addicted to coffee, I’m addicted to TikTok, or I can’t stop listening to this song on repeat. In a way, those statements aren’t wrong. Addiction, at its core, is the brain grabbing hold of something that makes it feel good and urging us to do it again. But, do it often enough, and the habit can start to tighten its grip.
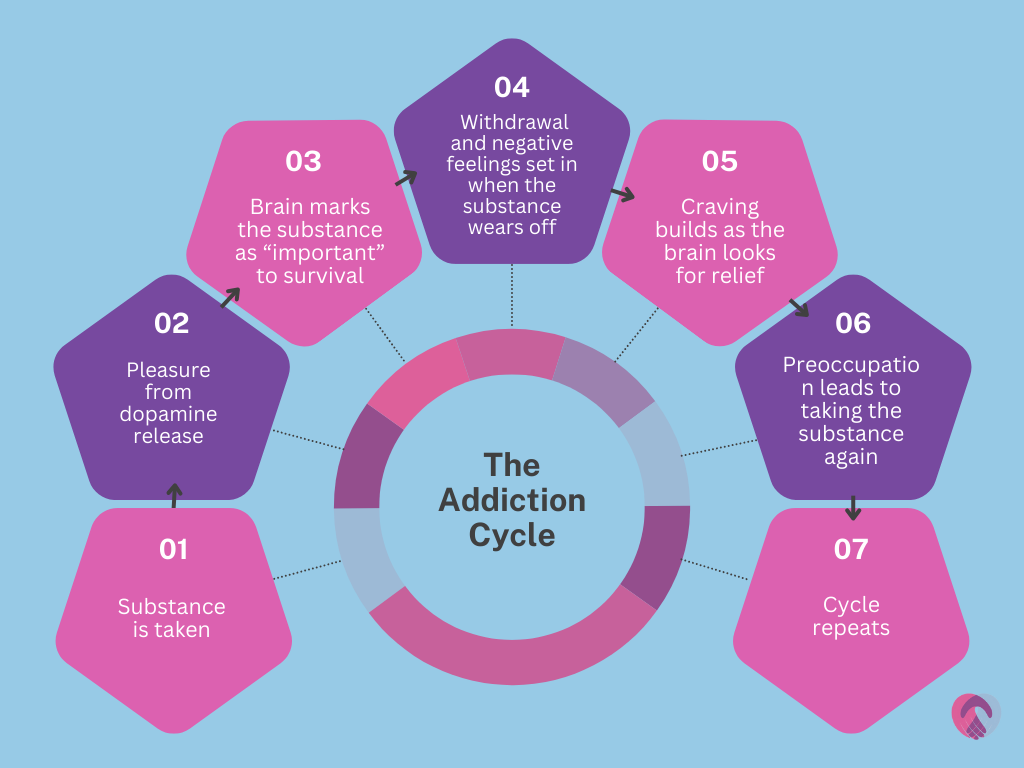
Neurologically, it plays out a bit like this:
While all addictions basically follow the same sort of cycle, different substances and behaviours have the potential to impact every part of a person’s life.
What are some of the most destructive types of addiction
When people picture addiction, the mind usually jumps to the heavy hitters: alcohol, drugs, maybe gambling or porn. These are the addictions with a reputation, known for how quickly they can strip life bare and demand more than anyone can give. Below, we break them down into key categories.
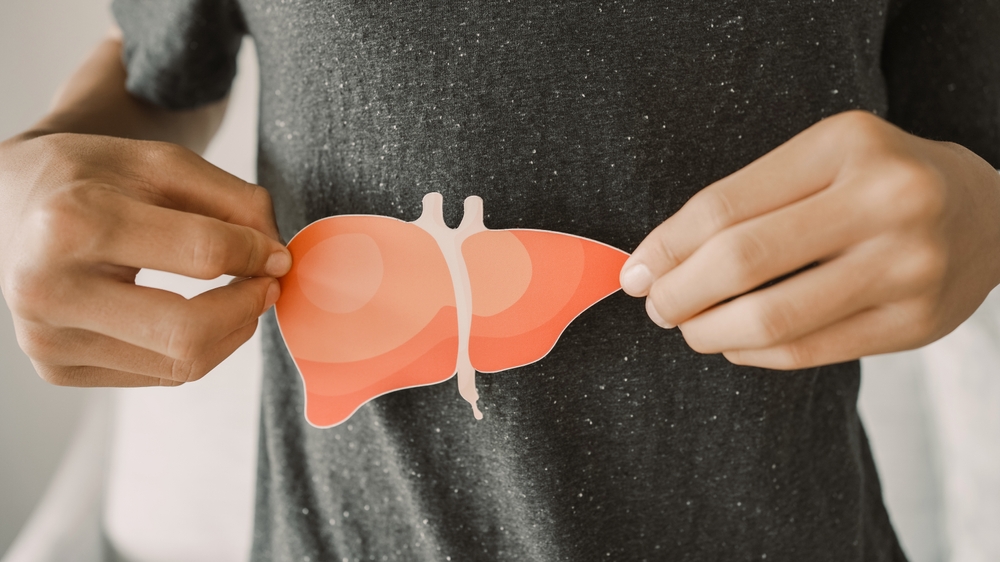
Alcohol addiction
With alcohol being legal in most countries, it can be easy to forget how powerful a substance it is. Here, we’re not talking about its immediate effects, like being very drunk, but the way it can become so addictive that stopping abruptly can cause seizures and even death.
Alcohol addiction
Drug addictions
Illegal substances might differ in the feelings they bring, but the outcome is often the same. Drugs like heroin or cocaine can take hold so quickly that life begins to revolve around use, and attempts to quit often trigger intense withdrawals that feel impossible to push through alone.
Drug addictions
Prescription drugs
When medication comes with a doctor’s note, it can feel safe. Painkillers such as oxycodone or sedatives like diazepam, however, can create a dependency that grows quietly. Stopping isn’t as simple as throwing the tablets away, as the body may react sharply when the supply suddenly ends.
Prescription drug addictions
Behavioural addictions
Behaviours like gambling or compulsive shopping don’t change the body in the same way substances do, yet they still have a powerful grip. The pull can become so strong that people spend money they don’t have or lose connection with others, finding it extremely difficult to break free.
Behavioural addictions
Legal high addictions
Sold under bright packaging or even in everyday shops, substances like Spice or nitrous oxide are often mistaken for safer options. The reality is different. These drugs can cause lasting mental and physical harm, and once dependence forms, stopping can feel just as challenging as with illegal substances.
Legal high addictions
What causes people to develop addictions?
If you asked most people why someone develops an addiction, the quick answers would be words like self-inflicted or lack of control. Those ideas have been floating around for decades, but they don’t really explain anything. Addiction isn’t solely focused on what some would perceive as “weakness”; rather, it’s a mix of forces that come together in different ways for different people.
Research over the years has dug into why some are pulled into addiction while others, even in the same environment, are not. There’s no single answer and no neat formula. What we can do, though, is look at the evidence and see the patterns that keep showing up.
Mental health difficulties
In many cases, addiction has been shown to correlate with certain mental health issues. The real question is which comes first. Did the mental health issue lead to the addiction, or did the addiction cause the mental health issue? It’s the chicken and the egg paradox, and the answer is rarely simple. What we do know is that the two often sit side by side, so looking at the research helps us understand how deep the connection really goes.
- In schizophrenia, around 4 in 10 people are also living with a substance use disorder.
- People with bipolar disorder face similarly high numbers, with 42% also struggling with alcohol problems and 20% with cannabis problems.
- Depression and substance use regularly appear side by side, too, with about 1 in 4 people with depression also having some form of addiction.
- Having an anxiety disorder roughly doubles your risk of alcohol dependence, and if you drink to cope, your chances of developing a serious alcohol problem shoot up even more.
Personality traits
Psychologists often talk about the “big five” personality traits: openness, conscientiousness, extraversion, agreeableness, and neuroticism. Studies have shown that these traits can play a part in how likely you are to develop, or stick with, an addiction. These traits don’t cause addiction by themselves, but they can tip the scales if put in a position to.
- People who score high in neuroticism and lower in conscientiousness or agreeableness are more likely to drink heavily or struggle to cut down.
- People who are more dutiful, thoughtful in their decisions, and open in how they deal with others tend to show lower rates of alcohol misuse. These traits act as a kind of buffer, making it easier to avoid slipping into harmful patterns.
- Struggling to wait for long-term rewards is strongly tied to addiction severity. Studies show that choosing a “smaller reward now” over a “bigger reward later” is common across alcohol, drugs, and gambling, with the effect even stronger in people already battling an addiction.
Environmental exposure
Growing up in a home or community where substances are common makes it far more likely that a person will experiment, and once exposure begins, the risk of addiction rises. Stress, trauma, or even just the availability of substances in your neighbourhood all add weight to the equation.
- More than half of people in addiction treatment report experiencing four or more adverse childhood experiences.
- Studies show that just having one adverse experience in childhood makes someone around four times more likely to develop an addiction later in life.
- In England, areas with the most alcohol outlets see far higher alcohol-related hospital admissions than areas with fewer outlets.
- For young people, peer groups are especially powerful: when fewer friends use substances, long-term abstinence rates are far higher; when many do, the odds of staying sober drop sharply.
Genetics
Genetics and the link to addiction is a complex, sometimes controversial, subject. Some argue genes are central, others believe the environment carries far more weight. The truth is probably somewhere in between. Genetics might load the dice, but it’s your experiences that decide how many times those dice get rolled.
- Alcohol use disorder is around 50% heritable in large twin and adoption studies.
- Research also shows that the same genes often increase risk across different substances, not just one, which helps explain why people often struggle with more than a single addiction at a time.
Do I have an addiction?
One of the hardest parts of addiction is recognising it in yourself. Many people brush off the signs as just a phase, stress, or something they’ll get on top of eventually. The truth is that addiction rarely announces itself loudly in the beginning. It creeps in, reshaping your habits, your thinking, and your relationships before you’ve even had the chance to notice.
That’s why it’s important to check in with yourself honestly. Not to shame or criticise, but to get a clearer picture of where you are. Addiction doesn’t always look like the stereotypes we’re used to seeing. For some people, it’s waking up and needing that first drink before the day can start. For others, it’s the compulsion to gamble until there’s nothing left in the bank. For some, it’s spending more time online than with the people they care about.
Ask yourself the following questions:
- Have I tried to stop but found I couldn’t?
- Do I feel anxious or low when I can’t use or do the behaviour?
- Is it affecting my health or the way I feel day to day?
- Have relationships started to suffer because of it?
- Do I spend more time thinking about it than anything else?
- Is it costing me more, financially, emotionally, or physically, than I ever expected?
If several of these questions ring true, it doesn’t mean you’re broken or beyond help. It simply means the line between use and dependency may already be blurred. The fact that you’re even questioning it is important. Most people caught in addiction go years without ever pausing to reflect. Taking a moment now to ask these questions could be the first step toward changing everything.
Are addictions treatable?
At UKAT, we know that addiction is treatable, and our centres across the UK are dedicated to proving that every day. We approach recovery by caring for both the body and the mind. For those struggling with substances, a medically managed detox is often the first step, creating the space for deeper therapeutic work to begin.
From there, our residential programmes combine evidence-based therapies with holistic support, helping you to address not just the addiction but also the underlying factors that fuel it. Each one of our centres provides a safe environment where you can fully focus on healing.
Importantly, recovery doesn’t end the moment you leave treatment. That’s why aftercare is built into what we do, ensuring you’re supported long after your stay. You’re not shown the back door and wished well; instead, you leave with guidance, connections, and a network to help you sustain long-term sobriety.
The message is clear: addiction is treatable. It isn’t easy, and it isn’t instant, but with the right help and the right environment, people rebuild their lives every single day.
What are the next steps?
If you’ve read this far, you’ve already taken an important step. Whether you’re worried about yourself or someone close to you, reaching out can feel daunting, but you don’t have to figure everything out before making contact.
The next step is to talk. At UKAT, our team is here to listen, answer your questions, and guide you through the options available. You might be calling for yourself, or you might be calling because you’re worried about a loved one. Either way, that call can be the turning point.
You don’t need to wait until things get worse. Even if you’re unsure whether it’s really an addiction or if you just want to explore what help looks like, speaking to us is a chance to find clarity. Contact us today and together, we can work out what’s happening and how to move forward.
Frequently Asked Questions
(Click here to see works cited)
- Semaan, Abdo, and Mashal K. Khan. “Neurobiology of Addiction.” PubMed, StatPearls Publishing, 2 Nov. 2023, www.ncbi.nlm.nih.gov/books/NBK597351/
- Hunt, Glenn E., et al. “Prevalence of Comorbid Substance Use in Schizophrenia Spectrum Disorders in Community and Clinical Settings, 1990–2017: Systematic Review and Meta-Analysis.” Drug and Alcohol Dependence, vol. 191, no. 191, Oct. 2018, pp. 234–58, https://doi.org/10.1016/j.drugalcdep.2018.07.011
- Anker, Justin. “Co-Occurring Alcohol Use Disorder and Anxiety: Bridging the Psychiatric, Psychological, and Neurobiological Perspectives.” Alcohol Research: Current Reviews, vol. 40, no. 1, 2019, https://doi.org/10.35946/arcr.v40.1.03 Accessed 17 Nov. 2019.
- Hakulinen, Christian, et al. “Personality and Alcohol Consumption: Pooled Analysis of 72,949 Adults from Eight Cohort Studies.” Drug and Alcohol Dependence, vol. 151, no. 1, June 2015, pp. 110–14, https://doi.org/10.1016/j.drugalcdep.2015.03.008
- Lui, P. Priscilla, et al. “Linking Big Five Personality Domains and Facets to Alcohol (Mis)Use: A Systematic Review and Meta-Analysis.” Alcohol and Alcoholism, vol. 57, no. 1, Apr. 2021, https://doi.org/10.1093/alcalc/agab030
- Amlung, Michael, et al. “Steep Delay Discounting and Addictive Behavior: A Meta-Analysis of Continuous Associations.” Addiction, vol. 112, no. 1, Sept. 2016, pp. 51–62, https://doi.org/10.1111/add.13535
- Madigan, Sheri, et al. “Adverse Childhood Experiences: A Meta‐Analysis of Prevalence and Moderators among Half a Million Adults in 206 Studies.” World Psychiatry, vol. 22, no. 3, Wiley-Blackwell, Sept. 2023, pp. 463–71, https://doi.org/10.1002/wps.21122
- Maheswaran, Ravi, et al. “Alcohol Outlet Density and Alcohol Related Hospital Admissions in England: A National Small-Area Level Ecological Study.” Addiction, vol. 113, no. 11, Aug. 2018, pp. 2051–59, https://doi.org/10.1111/add.14285 Accessed 29 Oct. 2019.
- Ivaniushina, Valeria, and Vera Titkova. “Peer Influence in Adolescent Drinking Behavior: A Meta-Analysis of Stochastic Actor-Based Modeling Studies.” PLoS ONE, vol. 16, no. 4, Apr. 2021, pp. 1–16, https://doi.org/10.1371/journal.pone.0250169
- Verhulst, B., et al. “The Heritability of Alcohol Use Disorders: A Meta-Analysis of Twin and Adoption Studies.” Psychological Medicine, vol. 45, no. 5, Aug. 2014, pp. 1061–72, https://doi.org/10.1017/s0033291714002165
- Miller, Alex P. “Generalized Genetic Liability to Substance Use Disorders.” the Journal of Clinical Investigation/the Journal of Clinical Investigation, vol. 134, no. 11, American Society for Clinical Investigation, June 2024, https://doi.org/10.1172/jci172881