“Coke nose” is a colloquial term used to describe the adverse effects on the nose resulting from the habitual use of cocaine. Cocaine is an extremely potent drug and its frequent insufflation (snorting) can have dire consequences on the nasal passages and surrounding structures. This can lead to a variety of symptoms and complications.
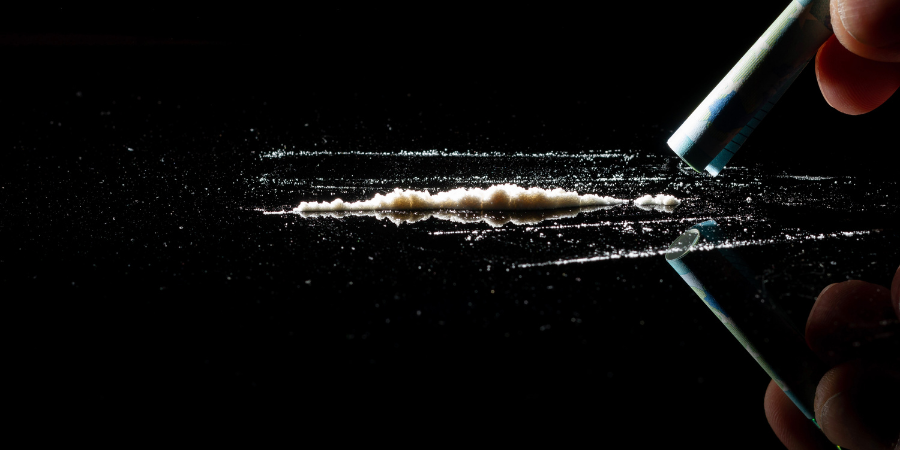
What is “Coke Nose”?
Coke nose is the informal term for a range of nasal problems caused by snorting cocaine. When cocaine is inhaled through the nose, it comes into direct contact with the nasal mucosa, which is the moist tissue lining the nasal passages. Cocaine is a potent vasoconstrictor, meaning it narrows blood vessels. This property contributes to its euphoric effects, but it also severely restricts blood flow to the delicate tissues inside the nose.
Causes of Coke Nose
The primary cause of coke nose is the frequent and prolonged use of cocaine. Here’s a detailed look at how this process works:
- Vasoconstriction: Cocaine’s vasoconstrictive properties reduce blood flow to the nasal tissues. Over time, this diminished blood flow can cause the tissues to become deprived of oxygen and nutrients, leading to necrosis (tissue death).
- Irritation and inflammation: Repeated exposure to cocaine irritates the nasal mucosa, causing chronic inflammation. This persistent irritation can damage the mucous membrane and underlying structures.
- Chemical toxicity: Cocaine itself is toxic to cells. Its direct contact with nasal tissues can cause cellular damage and death.
- Additives: Street cocaine is often cut with various substances that can exacerbate nasal damage. These adulterants can include anything from talcum powder to other drugs, each with its own potential to harm nasal tissues.
Symptoms of Coke Nose
The symptoms of coke nose can range from mild to severe and may progress with continued cocaine use. Common symptoms include:
Nasal congestion
- Description: Chronic stuffiness and congestion are often early signs of coke nose.
- Details: Users might find themselves frequently congested even when not using cocaine. This congestion occurs because cocaine causes the blood vessels in the nasal passages to constrict and then dilate, leading to swelling and inflammation of the nasal tissues. Over time, this repeated cycle can result in persistent congestion.
Nosebleeds (Epistaxis)
- Description: Frequent nosebleeds are a hallmark of coke nose.
- Details: The damaged and inflamed nasal tissues are more prone to bleeding, which can occur spontaneously or with minimal trauma. Cocaine irritates and damages the delicate lining of the nasal passages, making the blood vessels more susceptible to rupture. This can lead to regular nosebleeds that may vary in severity.
Nasal pain and discomfort
- Description: Persistent pain or a burning sensation in the nose is common.
- Details: This discomfort can be severe and may interfere with daily activities. The constant irritation and damage to the nasal tissues from cocaine use can result in chronic pain, which may be described as a burning, stinging, or aching sensation. The pain can become so intense that it distracts from normal activities and reduces the quality of life.
Loss of smell (Anosmia)
- Description: Damage to the olfactory receptors can lead to a diminished sense of smell.
- Details: This condition, known as anosmia, can affect the sense of taste as well since smell and taste are closely linked. Chronic cocaine use damages the olfactory receptors in the nasal passages, leading to a partial or complete loss of smell. This can significantly impact the user’s ability to enjoy food and detect odours, which can be dangerous in certain situations, such as not being able to smell smoke or gas leaks.
Crusting and scabbing
- Description: Chronic irritation can cause the nasal tissues to form crusts and scabs.
- Details: These crusts and scabs can be painful and prone to bleeding. As the nasal lining continues to be damaged by cocaine, it attempts to heal itself by forming scabs and crusts. These can cause significant discomfort and pain, especially if they are picked at or dislodged, leading to further bleeding and irritation.
Nasal septum perforation
- Description: In severe cases, the nasal septum can develop a hole, known as septal perforation.
- Details: This can cause a whistling sound when breathing and may lead to further complications. The nasal septum, composed of cartilage and bone, separates the two nostrils. Chronic cocaine use can erode this structure, creating a perforation. This not only causes a whistling sound during breathing but can also lead to infections, crusting, and further nasal deformities.
Saddle nose deformity
- Description: Extreme tissue loss can cause the collapse of the nasal bridge.
- Details: This leads to a visible indentation known as a saddle nose deformity, which is a severe and often irreversible condition. The extensive damage to the cartilage and bone of the nasal septum can result in the collapse of the nasal bridge. This deformity not only affects the appearance but can also impair nasal function, leading to breathing difficulties and chronic sinus issues. Surgical intervention is often required to attempt to correct this deformity, but complete restoration is not always possible.
These symptoms highlight the extensive and often irreversible damage that chronic cocaine use can cause to the nasal structures. Early intervention and cessation of cocaine use are crucial to prevent the progression of these symptoms and to preserve nasal function and structure.
Diagnosis of coke nose
Diagnosing “coke nose,” a condition resulting from chronic cocaine use, involves a comprehensive assessment combining patient history, physical examination, imaging studies, and laboratory tests. Here’s an expanded approach to diagnosing this condition:
-
Patient history
Drug use history:
- Inquiring about cocaine use: Detailed questioning about the patient’s history with cocaine, including the duration and frequency of use, the amount typically used, and any changes in patterns of use.
- Method of intake: Understanding whether the patient inhales, snorts, or uses cocaine through other routes (e.g., smoking or injecting) as the method of intake can impact the type and extent of nasal damage.
Symptom onset and duration:
- Symptom history: Gathering information about when the symptoms started, how they have progressed over time, and any factors that exacerbate or alleviate the symptoms.
- Associated symptoms: Asking about other related symptoms such as nasal congestion, nosebleeds, nasal pain, facial pain, or a decrease in the sense of smell.
-
Physical examination
Nasal examination:
- Inspection tools: Utilising an otoscope or nasal speculum to inspect the nasal passages for visible signs of damage.
- Visible damage: Looking for signs such as redness, swelling, and discharge, which may indicate infection or inflammation.
Septal perforation:
- Hole in the septum: Carefully checking for the presence of perforations in the nasal septum, which are often a direct result of chronic cocaine use.
- Size and location: Assessing the size and exact location of any perforations, as larger or more centrally located perforations may require different management strategies.
Mucosal health:
- Inflammation and ulceration: Assessing the condition of the nasal mucosa for signs of inflammation, ulceration, crusting, or atrophy.
- Crusting and dryness: Noting any crusting or excessive dryness of the nasal mucosa, which can be indicative of chronic irritation and damage.
-
Imaging studies
CT scan or MRI:
- Detailed imaging: Conducting a CT scan or MRI to obtain detailed images of the nasal and sinus structures. These imaging studies can help evaluate the extent of damage, detect any hidden infections, and assess the overall structural integrity.
- Sinus involvement: Identifying any involvement of the sinus cavities, including sinusitis or erosion of the sinus walls.
Endoscopy:
- Direct visualisation: A nasal endoscope is used to provide a more detailed visualisation of the nasal passages and deeper structures, including the sinus openings.
- Identifying abnormalities: Inspecting for signs of chronic inflammation, polyps, or other abnormalities that may not be visible through a standard nasal examination.
-
Laboratory tests
Toxicology screen:
- Substance detection: Conducting a toxicology screen to detect the presence of cocaine and other substances in the patient’s blood or urine. This can help confirm recent cocaine use and identify any co-occurring substance use.
- Metabolite analysis: Analysing the specific metabolites of cocaine to understand the timing and extent of recent use.
-
Additional considerations
Referral to specialists:
- Otolaryngologist (ENT): Referring the patient to an ENT specialist for a more detailed evaluation and management plan, especially if significant nasal damage or complications are present.
- Addiction specialist: The patient will then connect with an addiction specialist or counsellor to address the underlying substance use disorder and provide support for cessation and recovery.
Patient education and support:
- Informing about risks: Educating the patient about the risks of continued cocaine use, including the potential for further nasal damage, systemic health issues, and the importance of cessation.
- Support services: Providing information about available support services, including addiction treatment programmes, support groups, and medical follow-up for ongoing care.
By combining these diagnostic steps, healthcare providers can comprehensively assess the extent of nasal damage caused by chronic cocaine use, provide appropriate medical management, and support the patient in addressing their substance use disorder.
Treatment of coke nose
Treating “coke nose,” which is nasal damage caused by chronic cocaine use, requires a multifaceted approach addressing both the physical damage to the nasal structures and the underlying substance use disorder. Here’s a detailed outline of the treatment strategies:
-
Cessation of cocaine use
Preventing further damage:
- Immediate cessation: Stopping cocaine use is the most crucial step in preventing additional damage to the nasal passages and promoting healing.
- Counselling and Support: Engaging the patient in counselling and support services to address the psychological aspects of addiction.
Substance abuse treatment programmes:
- Inpatient and Outpatient programmes: Providing options for inpatient or outpatient treatment programs depending on the severity of the addiction and the patient’s needs.
- Behavioural Therapy: Utilising cognitive-behavioural therapy (CBT), motivational interviewing, and other evidence-based therapies to help the patient develop coping strategies and prevent relapse.
- Support groups: Encouraging participation in support groups such as Narcotics Anonymous (NA) for peer support and shared experiences.
-
Medical treatment
Saline nasal irrigation:
- Moisturisations: Using saline nasal sprays or irrigation systems (e.g., neti pots) to keep nasal passages moist and help remove debris and crusting.
- Regular use: Advising patients to perform nasal irrigation regularly to maintain mucosal health and prevent infections.
Topical antibiotics:
- Secondary infections: Topical antibiotics are prescribed to treat secondary bacterial infections that may occur due to damaged nasal mucosa.
- Application: Providing instructions on the proper application of topical antibiotics to ensure effectiveness.
Nasal steroids:
- Reducing inflammation: Using nasal steroid sprays to reduce inflammation and swelling of the nasal passages.
- Monitoring: Regular follow-up to monitor the patient’s response to treatment and adjust dosages as needed.
Pain management:
- Analgesics: Prescribing appropriate analgesics to manage nasal pain, taking into account the patient’s history of substance use and potential for abuse.
- Non-opioid options: Considering non-opioid pain management options such as acetaminophen or NSAIDs to avoid the risk of addiction.
-
Surgical intervention
Septal perforation repair:
- Indications for surgery: Consider surgical repair for severe septal perforations that cause significant symptoms or complications.
- Surgical techniques: Techniques such as septal button placement or autologous grafting are employed to repair the perforation.
Reconstructive surgery:
- Structural damage: Addressing significant structural damage, such as saddle nose deformity, through reconstructive surgery.
- Preoperative evaluation: Conducting thorough preoperative evaluation and planning to ensure optimal outcomes.
- Postoperative care: Providing detailed postoperative care instructions to promote healing and prevent complications.
-
Additional considerations
Multidisciplinary approach:
- Collaboration: Involving a team of healthcare providers, including primary care physicians, ENT specialists, addiction specialists, and mental health professionals, to provide comprehensive care.
- Integrated care: Ensuring integrated care that addresses both the physical and psychological aspects of the patient’s condition.
Patient education and support:
- Informing about risks: Educating the patient about the risks of continued cocaine use and the importance of cessation for nasal and overall health.
- Support services: Providing information about available support services, including addiction treatment programs, support groups, and medical follow-up for ongoing care.
Long-term monitoring:
- Regular follow-up: Scheduling regular follow-up appointments to monitor the patient’s progress, manage any complications, and support their recovery journey.
- Relapse prevention: Implementing strategies for relapse prevention, including ongoing counselling, support group participation, and medication management if necessary.
By addressing both the immediate physical damage and the underlying addiction, this comprehensive treatment approach aims to promote healing, prevent further damage, and support long-term recovery for individuals suffering from coke nose.
Preventing coke nose
Preventing “coke nose” involves harm reduction, medical intervention, and, ideally, cessation of use. Harm reduction strategies include minimising use, staying hydrated, using saline nasal sprays and lubricants, avoiding sharing snorting devices, and ensuring a clean environment. Medical intervention, such as regular check-ups with an ENT specialist and seeking professional medical advice, can majorly help manage and mitigate damage.
The most effective prevention is stopping cocaine use. This can be achieved through professional help, support groups like Narcotics Anonymous, behavioural therapies such as Cognitive Behavioral Therapy (CBT), and, in some cases, medication. Adopting a healthy lifestyle with a balanced diet, regular exercise, and stress management can support recovery. If symptoms of “coke nose” appear, it’s crucial to cease cocaine use immediately and seek medical attention to prevent further damage.
Do you need help with cocaine addiction?
If you or someone you know is struggling with cocaine addiction, don’t wait—seek help now. Contact UKAT today. Your path to recovery and a healthier life starts with taking the first step. Reach out and reclaim your future.





