Last Updated:
March 28th, 2025
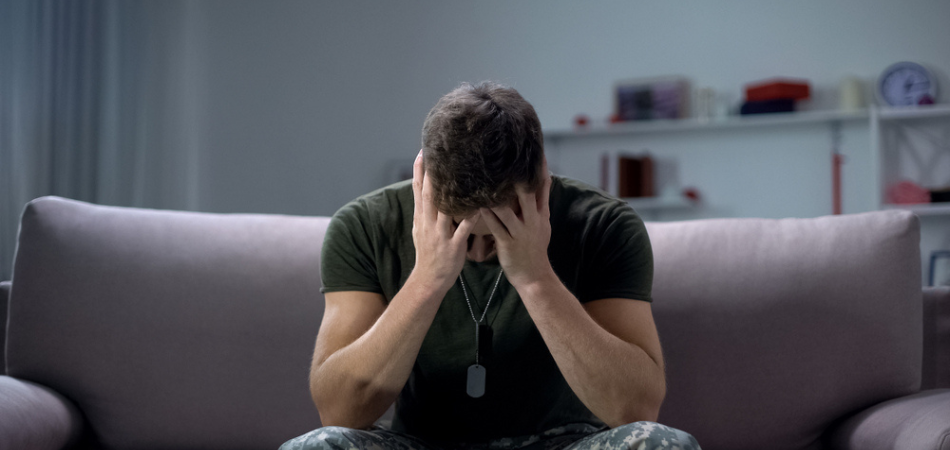
Veterans coming home from service tend to face extremely unique challenges. These aren’t limited to what one might typically expect of highly-charged combat environments (namely, physical injuries). In fact, invisible wounds sustained from war are far more common for returning soldiers.
Mental health issues like post-traumatic stress disorder (PTSD), depression and anxiety are the most frequently observed conditions among those who have experienced prolonged deployment or intense combat scenarios. These psychological issues can – and often do – lead to substance use disorders (SUD), with many veterans turning to drugs and/or alcohol as coping mechanisms for their trauma.
Below, we will explore the connection between trauma and addiction among veterans, looking particularly at the underlying cause, impact on their lives, and recovery procedures.
Why veterans are susceptible to trauma and PTSD
Veterans experience trauma at a higher rate than most people. This trauma is normally catalysed by combat, military sexual assaults, and the consistent, almost never-ending threat of danger. In turn, such catalysts increase the risk of developing PTSD. The chronic stress and constant adrenaline linked to these experiences can lead to permanent and lasting changes in brain chemistry and function.
Veterans may turn to alcohol or drugs as a means of self-medicating to alleviate symptoms of PTSD, such as hypervigilance, nightmares, and anxiety. This coping mechanism, while temporarily providing relief, can lead to alcohol addiction or drug addiction.
The combination of PTSD and addiction severely impacts a veteran’s mental health, leading to a range of issues, including worsened depression, anxiety, and increased risk of suicide. The use of substances to cope with trauma can worsen PTSD symptoms over time and lead to a deteriorating mental health condition that requires genuine treatment.
Statistics on the subject of veterans facing trauma and PTSD
Approximately 11% of veterans seeking initial care meet the criteria for a substance use disorder. The link between PTSD and SUD is quite alarming, with 63% of recent Iraq and Afghanistan veterans diagnosed with SUD also meeting the criteria for PTSD , according to the National Institute on Drug Abuse. This tends to worsen the challenges faced by veterans, leading to poorer treatment outcomes.
Alcohol misuse is also very common, with veterans exhibiting higher instances of heavy drinking compared to non-veterans. Over 56% of veterans reported alcohol use in a one-month period, and about 11% of those seeking treatment were driven by heroin addiction. These behaviours are often linked to the stressors of deployment, such as separation from loved ones, exposure to life-threatening situations, and the pressure of difficult missions.
Challenges that veterans face during treatments for trauma, PTSD, and related drug issues
There is a multifaceted amount of issues veterans may face when it comes to seeking addiction and mental health help. Some examples can include:
- Access to care: Veterans often face significant challenges in accessing the care they need for trauma, PTSD, and related substance use disorders. A critical issue is the availability of services, particularly in rural areas where there is often a shortage of mental health professionals trained to handle these specific conditions. Long wait times at Veterans Affairs (VA) facilities further exacerbate this problem, leaving many veterans without timely access to necessary treatments. Additionally, geographical barriers pose a substantial challenge, as many veterans live far from VA facilities or specialised treatment centres, making it difficult for them to attend regular appointments and receive continuous care.
- Stigma and cultural barriers: Stigma and cultural barriers significantly impact veterans seeking treatment for mental health issues. There is a pervasive stigma associated with mental health conditions within both society and the military, where these issues can be perceived as signs of weakness. The military culture, which emphasises toughness and self-reliance, often discourages veterans from admitting to psychological problems and seeking help. Furthermore, there are widespread misunderstandings about PTSD and substance use disorders, which can lead to misconceptions and judgments from peers and family members, further deterring veterans from pursuing the help they need.
- Financial and logistical issues: Financial and logistical issues present substantial barriers for veterans seeking treatment for PTSD and substance use disorders. Even with VA benefits, some treatments can carry associated costs that may be prohibitive for veterans. Those who seek care outside the VA system may encounter issues with insurance coverage, leading to additional out-of-pocket expenses. Moreover, the financial strain of being unable to work due to mental health or substance use issues can complicate the treatment process. This lack of financial stability can make it difficult for veterans to prioritise their health and consistently engage in necessary treatments.
- Quality of care: The quality of care that veterans receive for PTSD and substance use disorders can vary widely, impacting their recovery outcomes. Continuity of care is often disrupted due to transitions between providers or changes in treatment plans, leading to gaps in treatment. Not all veterans receive evidence-based treatments, which are critical for effective recovery, and this inconsistency can hinder progress. Additionally, there is often a lack of holistic care that addresses both mental health and substance use issues simultaneously, resulting in fragmented treatment approaches that fail to consider the interconnected nature of these conditions.
- Co-occurring conditions: Veterans frequently present with complex medical histories that include multiple co-occurring conditions, such as chronic pain, traumatic brain injury (TBI), and depression, which complicate treatment for PTSD and substance use disorders. Coordinating care for these conditions can be challenging, especially when services are fragmented across different providers. This lack of integrated care can lead to ineffective treatment strategies and poorer outcomes, as the interplay between physical health, mental health, and substance use is not adequately addressed in a cohesive manner.
- Psychological and emotional barriers: Psychological and emotional barriers significantly impede veterans’ ability to engage in treatment for PTSD and substance use disorders. Trauma-related symptoms, such as hypervigilance, flashbacks, and avoidance, can make it difficult for veterans to participate fully in therapeutic interventions. Trust issues are also common, as past negative experiences with healthcare providers can lead to a reluctance to seek help or fully engage in treatment. Furthermore, maintaining motivation and engagement in treatment is particularly challenging for those with severe symptoms, as the daily struggle with these conditions can erode the determination needed to adhere to treatment plans.
- Support systems: The presence or absence of support systems plays a crucial role in the recovery of veterans dealing with PTSD and substance use disorders. Many veterans experience social isolation, lacking the network of support that is essential for emotional and practical assistance during treatment. Family dynamics can also be strained, as family members are often affected by the veteran’s condition, adding stress and complicating the treatment process. Enhancing support networks through family support programmes and community-based initiatives can provide the necessary backing that veterans need to navigate their recovery journey successfully.
- Legal and criminal justice issues: Veterans with substance use disorders often face legal and criminal justice issues that complicate their ability to receive treatment. Legal problems related to substance use can create additional barriers, such as court obligations or incarceration, which interrupt treatment plans and hinder recovery efforts. Moreover, having a criminal record can limit access to certain types of treatment and support services, making it more difficult for veterans to find and engage in effective care. Addressing these legal and criminal justice issues through supportive legal services and alternative sentencing programs can help veterans stay on track with their treatment and improve their chances of recovery.
The treatments available for these conditions are varied and continuously evolving. However, many veterans still face a range of issues when undergoing these treatments. Here are some examples of common treatment options.
- Psychotherapy
Trauma-focused psychotherapies, such as Cognitive Processing Therapy (CPT), Prolonged Exposure (PE), and Eye Movement Desensitisation and Reprocessing (EMDR), are considered the gold standard for treating PTSD. These therapies help veterans process traumatic memories and reduce symptoms by addressing the psychological impact of trauma directly. Many veterans may find treatments like this emotionally taxing and challenging to complete due to the intensity of revisiting traumatic events. It’s important to find a healthcare provider that is tuned to and trained specifically in veteran-based psychotherapy.
- Medications
Pharmacotherapy is another key part of PTSD treatment. Four primary medications are recommended for PTSD. These are:
- Paroxetine
- Mirtazapine
- Amitriptyline
- Phenelzine
- Other therapies
Recent advancements include the use of virtual reality therapy, which immerses veterans in controlled, simulated environments to help them confront and process traumatic experiences safely. This method has shown promise in reducing PTSD symptoms and improving patient engagement. Another emerging treatment is Transcranial Magnetic Stimulation (TMS), which uses magnetic fields to stimulate nerve cells in the brain and has shown positive results in reducing PTSD symptoms among veterans.
Get the right help today
At UKAT, we offer addiction and mental health support tailored to the unique needs of veterans. If you or a loved one is struggling with addiction or mental health issues, our specialised treatments and compassionate care can help guide you towards recovery.