Last Updated:
March 28th, 2025
According to a recent study that analysed 19 years’ worth of data, England’s battle against dihydrocodeine abuse has been well underway for many years. Considered a ‘weak’ opioid by pharmacological standards, the study has called for an urgent re-evaluation of how we view dihydrocodeine and its potentially destructive properties.
In this blog, we’ll dive straight into exactly what dihydrocodeine is, how and when it’s used, the chances of addiction, and what to do next if you feel as though you’re becoming dependent on dihydrocodeine.
What is dihydrocodeine?
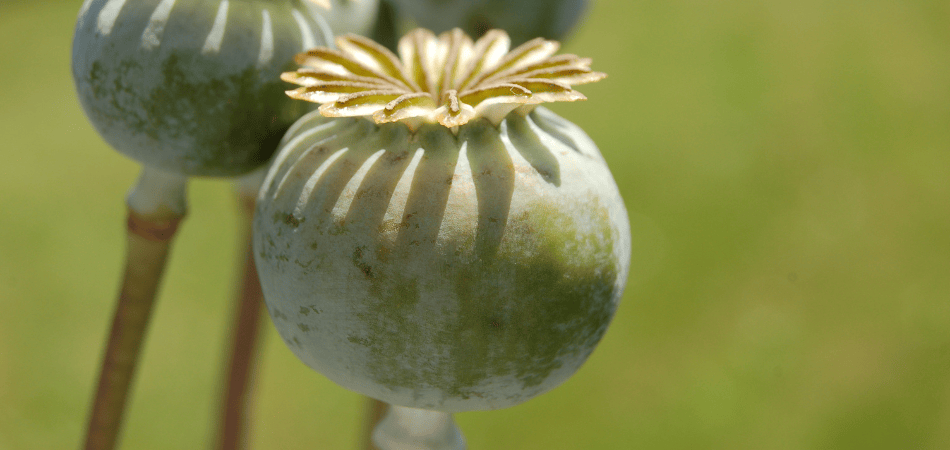
Dihydrocodeine is a semi-synthetic opioid derived from codeine, a naturally occurring alkaloid found in opium poppies. While its origins lie in the opium poppy plant, dihydrocodeine is typically synthesised through chemical processes, making it a semi-synthetic drug.
Classification-wise, dihydrocodeine is categorised as an opioid analgesic. These substances work by binding to opioid receptors in the central nervous system, thereby altering the perception of pain. It is considered a Class B substance in the UK due to its potential for abuse and dependence, requiring a prescription for legal use. Dihydrocodeine is considered to be twice as potent as codeine.
When is dihydrocodeine used?
Dihydrocodeine has a specific place in the broader landscape of pain management. It is used to provide relief for moderate to severe pain. Here’s how it fits into the larger context of pain management:
| Indication | Description |
|---|---|
| Moderate to severe pain | Prescribed when non-opioid pain relievers are inadequate for managing pain. Used for more intense pain. |
| Post-surgery or trauma | Prescribed for acute pain, such as post-surgery recovery or after traumatic injuries for short-term use. |
| Chronic pain management | Considered for chronic pain conditions like cancer-related pain, under close medical supervision and part of a comprehensive pain management plan. |
| Opioid rotation | Used when a patient’s current opioid medication is less effective, may be switched to dihydrocodeine or another opioid to improve pain control. |
| Balancing Benefits and Risks | Prescribers assess pain and weigh benefits against the risks (tolerance, dependence, side effects) before prescribing. |
Information taken from; NHS, Faculty of Pain Medicine and NCBI
How does dihydrocodeine work?
Dihydrocodeine works by binding to specific opioid receptors in the brain and spinal cord. These receptors are part of the central nervous system’s pain-regulating network. When dihydrocodeine binds to these receptors, it triggers a number of events that ultimately modulate the perception of pain. It interferes with the pain signals along neural pathways, reducing the sensation of discomfort.
It is important to note that dihydrocodeine comes with the risk of tolerance, dependence, and potential side effects. Therefore, its use should be closely monitored by healthcare professionals, and it should be taken strictly as prescribed.
Legality in the UK
In the UK, dihydrocodeine is only available via prescription if the tablet contains only dihydrocodeine and no other active ingredients. When it comes to over-the-counter products containing the drug, there are some set rules:
- Regulated pharmacies can sell certain over-the-counter medications containing dihydrocodeine without a prescription. These could be products with other pain relievers like paracetamol and aspirin.
- One over-the-counter product containing 7.46 mg of active ingredient is allowed.
- Customers can only buy one pack of 32 tablets at a time unless the pharmacist approves more.
- These products can be displayed and advertised to customers under the supervision of a pharmacist and must include a warning about the risk of addiction on the packaging.
The dark side of dihydrocodeine
Dihydrocodeine, like many opioids, carries a notable risk of addiction. In 2022, a comprehensive investigation was conducted to analyse mortality data associated with dihydrocodeine usage in England. The study spanned a 19-year period from 2001 to 2020. The findings derived from this study yielded multiple key insights.
- A total of 2,071 fatalities were attributed to dihydrocodeine use.
- The highest incidence of fatalities was linked to the unauthorised acquisition of dihydrocodeine.
- Accidental deaths resulting from dihydrocodeine misuse within the context of polypharmacy are on the rise.
- The perception of dihydrocodeine as a low-potency opioid might contribute to inadvertent overdosing.
- Individuals with intentions of self-poisoning are specifically seeking over-the-counter dihydrocodeine.
- There is a pressing need for a review of easily accessible over-the-counter opioid preparations.
So, what factors are contributing to addiction and overdoses? In the next section, we delve deeper into these potential factors.
Factors contributing to addiction
Understanding the factors contributing to addiction and recognising signs of addiction and dependence is crucial for both healthcare professionals and patients.
Dihydrocodeine’s potential for addiction lies in its ability to create a sense of euphoria and relief from pain. As users develop a tolerance to the drug, they may require higher doses to achieve the same effect. This tolerance can quickly lead to physical and psychological dependence.
Several factors contribute to the risk of addiction associated with dihydrocodeine, including:
- Genetics: Some individuals may be genetically predisposed to a higher risk of addiction when exposed to opioids like dihydrocodeine.
- Psychological factors: Co-existing mental health issues, such as depression or anxiety, can increase the vulnerability to addiction.
- Social environment: A person’s social and familial environment can play a significant role. Exposure to substance abuse within someone’s social circle can influence addiction.
- Length and dosage of use: The longer dihydrocodeine is used and the higher the dosage, the greater the risk of developing dependence.
Recognising signs of addiction and dependence
It’s essential to be vigilant and recognise signs of addiction and dependence in oneself or others. These signs may include:
Craving for the drug: An intense desire for dihydrocodeine, even when it’s not required for pain relief.
Loss of control: An inability to limit or control dihydrocodeine use, even when aware of its negative consequences.
Withdrawal symptoms: Physical and psychological distress when not using dihydrocodeine. These could include the following:
- Flu-like symptoms
- Muscle aches and pains
- Gastrointestinal distress
- Sweating
- Anxiety and restlessness
- Mood changes
- Increased heart rate and blood pressure
- Dilated pupils
Neglecting responsibilities: Neglecting daily obligations and responsibilities due to dihydrocodeine use.
Continued use despite harm: Continued use despite negative consequences, such as health issues or strained relationships.
Recognising these signs early and seeking help from healthcare professionals is crucial for preventing the progression of addiction and promoting effective pain management strategies that minimise risk.
Recognising the red flags of dihydrocodeine use
If you’ve been prescribed dihydrocodeine for pain management, it’s important to periodically ‘check in’ with your usage to ensure that you’re not unintentionally slipping into addiction. Additionally, for those who have been using this drug recreationally, it’s crucial to assess your usage as well. Here are six questions to help you gauge whether your dihydrocodeine use may be problematic:
- Have you been taking dihydrocodeine more frequently or in higher doses than prescribed or recommended?
- Do you find yourself constantly thinking about or craving dihydrocodeine, even when you don’t have a medical need for it?
- Have you experienced negative consequences in your personal or professional life as a result of your dihydrocodeine use?
- Are you experiencing withdrawal symptoms such as nausea, sweating, or irritability when you try to reduce or stop your dihydrocodeine use?
- Have you tried unsuccessfully to cut down or quit using dihydrocodeine on your own?
- Have you ever “doctor-shopped” or obtained dihydrocodeine from multiple healthcare providers to obtain larger quantities? (USA specific)
If you or someone you know answers “yes” to these questions, it may indicate a potential issue with dihydrocodeine abuse or dependence, and it’s important to seek help and support from a healthcare professional.
How can I get help for dihydrocodeine addiction?
UKAT offers a specialised in-house rehabilitation programme tailored for opioid addiction, including dihydrocodeine. This programme is designed to provide comprehensive support for people struggling with the challenges of opioid dependence.
UKAT’s in-house rehabilitation programme includes elements such as detox, counselling, therapy and aftercare planning to ensure long-term recovery success.
One of the key advantages is the availability of help 24/7 within this in-house programme. This round-the-clock accessibility ensures that you can access care and support whenever you need it, even during emergency situations.
Crucially, UKAT’s team of healthcare professionals and addiction specialists brings a wealth of experience to the table. Our expertise in addiction treatment means that you will receive expert care, support and guidance throughout your journey to recovery.
What are the next steps?
Taking the first step to reach out for the right support is crucial in breaking free from the cycle of addiction and embarking on a path towards a healthier, substance-free life. It’s important to remember that seeking help is a display of strength, and with the appropriate support and treatment, recovery is possible and achievable.
Contact UKAT today to initiate your journey to overcome your dihydrocodeine addiction.